5 Factors Influencing Informal Caregiver Burnout
Explore caregiver burnout through a new evidence-based framework that honours the complex emotional, relational, and systemic realities of informal caregiving. Such as caregiving volunteers who love someone but are not paid for their care.
Grounded in psychology, written for caregivers and those who support them. The Model (ICIM) considers the unique experience of each caregiver, what they’re carrying, and how the systems around them shape their experience. This is validating for caregiver burnout and attends to the broader context of identity.
Caregiver Burnout is Real
Burnout usually shows up first as a slow erosion of energy, lack of clarity or brain-fog, identity confusion, or loss of hope. For years, the primary language we’ve used to describe this experience has been the “burden” of caregiving. But what if that word doesn’t capture the whole story?
Recent research suggests we need a more nuanced framework, one that reflects the reality many caregivers already feel: this is hard and it’s burning me out. That’s part of how I came up with my 4-phase burnout recovery model that works not only for professionals and executives in burnout, but for family caregivers too.
Caregiver Burnout Isn’t Just a Work Problem
Burnout has traditionally been studied in formal workplace settings. But family caregiving isn’t a job that ends at 5:00. It’s intimate, ongoing, often invisible. Gérain and Zech (2019) argue that burnout applies deeply to informal caregivers family members, friends, and others who offer essential care outside of paid employment and they often don’t have the resources for stay well.
Burnout in caregivers includes three parts:
1. Emotional exhaustion: feeling drained and unable to keep giving emotionally.
2. Depersonalization: a growing distance or numbness in the relationship with the care recipient.
3. Reduced personal accomplishment: the fading sense that caregiving is meaningful or valued.
These are natural human responses to sustained emotional strain.
Why “Burden” Doesn’t Tell the Whole Story
“Burden” has long been used to measure the impact of caregiving. But as Gérain and Zech point out, it’s a vague and inconsistent concept. Sometimes it refers to physical strain, other times emotional distress or financial pressure. Because it lacks clarity, it can be hard to use as a foundation for meaningful support.
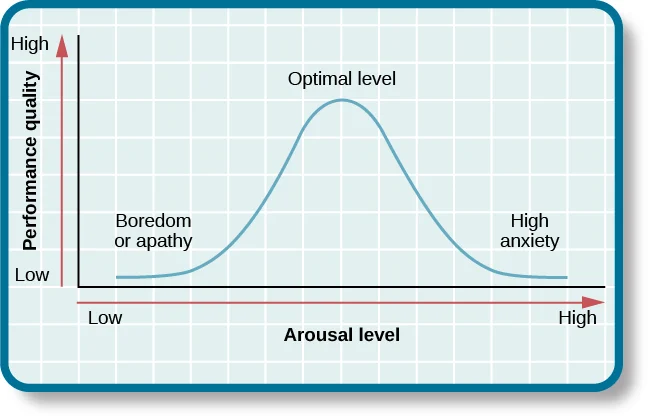
Instead, the researchers suggest that burden is best understood as subjective appraisal: how a caregiver interprets and feels about the challenges they face. It’s not the situation alone that creates strain, but the meaning we make of it, especially when resources are low or when we feel alone in the task. It’s important to trust the caregivers own assessment of how they are and what the experience is giving to them or costing them.
5 Factors to Understand Caregiver Burnout
The researchers propose a new model called the Informal Caregiving Integrative Model (ICIM). This model considers who caregivers are, what they’re carrying, and how the systems around them shape their experience. It honours that there are many factors at play that influence caregiver burnout.
5 Key aspects of the informal caregiving model include:
1. Personal characteristics: Emotional regulation, coping style, physical health, and prior roles (like parenting or employment) all influence vulnerability to caregiver burnout.
2. The caregiving setting: Who you’re caring for, how intense their needs are, and what caregiving looks like day-to-day matter but so do the side effects like lost sleep, social isolation, or family conflict.
3. Social and cultural environment: Support from partners, family, and professionals can buffer or intensify strain. Cultural beliefs about caregiving like the pressure to “do it all” or keep things private can make burnout harder to recognize or name.
4. Appraisal: Your personal interpretation of stress, whether positive or negative, has real consequences. Seeing caregiving as meaningful may help with resilience.
5. Relationship quality: One of the most overlooked variables. When caregiving changes the dynamic between two people, that shift can be a source of grief, guilt, or distance, even though love remains.

Caregiver Burnout is Real
Caregiver burnout has physical, emotional, and social consequences. Research shows that burnout can lead to anxiety, depression, withdrawal, poorer physical health, and increased risk of hospitalization for both the caregiver and the person receiving care (Gérain & Zech, 2019). When left unaddressed, burnout also increases the chance of institutionalization or unintentional neglect for recipients.
It’s about limits. And every human being has them.
Toward More Honest Conversations
What this model makes clear is that we need to stop oversimplifying the caregiving experience. Burnout is about carrying too much without enough support, acknowledgment, or space to feel. The Mayo clinic has a helpful article on how to manage caregiver stress, click here.
What helps with Caregiver Burnout?
– Support systems that are relational, not transactional.
– Language that includes both pain and purpose – spiritual conversations.
– Intervention tools that reflect the complexity of real-life caregiving.
– And safe spaces, whether in therapy, community, or personal reflection, where caregivers can lay their burdens down and feel validated and understood, even for a moment.
If you are experiencing caregiver burnout, and you feel lost, exhausted, or alone, know this: the research is catching up to your reality. Your story is valid and your well-being matters not just for the person you’re helping, but for you. Reach out for a free 20-minute conversation and get support.
What Happens in a Free Consult?
Your 20 minute consult is a no-pressure conversation.
– Talk about what’s weighing on you
– Learn how I approach recovery and what sessions will be like
– Decide if we’re the right fit
You’ll leave with clarity on your next step, whether we work together or not.
References
Gérain, P., & Zech, E. (2019). Informal Caregiver Burnout? Development of a Theoretical Framework to Understand the Impact of Caregiving. Frontiers in Psychology, 10, 1748. https://doi.org/10.3389/fpsyg.2019.01748
For clients in Saskatchewan, visit the spiritual psychotherapy page here.